Is HER2 positive cancer curable?
2024-05-07
By admin
Understanding HER2 Positive Cancer
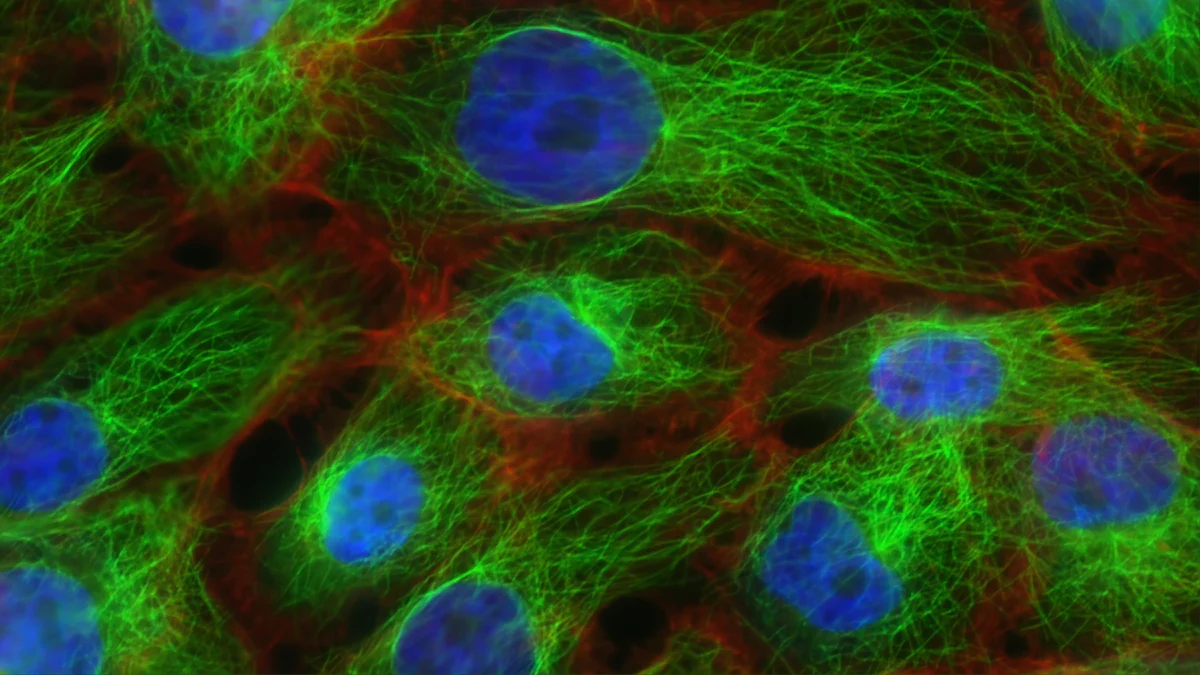
HER2 positive cancer refers to a specific type of cancer that is characterized by the overexpression of the HER2 protein. The HER2 gene is responsible for providing instructions for making the HER2 neu protein, which plays a crucial role in the growth and division of cells. When there is an excess of HER2 neu protein in cancer cells, it can lead to uncontrolled cell growth and proliferation, contributing to the aggressive nature of the cancer.
What Does HER2 Positive Mean?
The Role of HER2 in Cancer
The overexpression of HER2 can significantly influence the behavior of cancer cells. It can make the cancer more likely to spread and less responsive to hormone therapy. This aggressive behavior makes HER2 positive cancers more challenging to treat compared to other types of breast cancers.
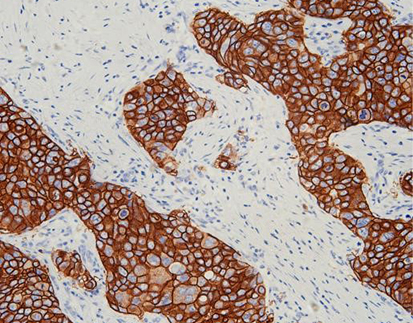
Identifying HER2 Positive Cancer: HER2 IHC and Other Tests
Healthcare providers use various tests to identify whether a cancer is HER2 positive. One common test is immunohistochemistry (IHC), which assesses the levels of HER2 neu protein on the surface of cancer cells. Additionally, fluorescence in situ hybridization (FISH) may be used to analyze the genetic material within cancer cells.
The Impact of HER2 on Breast Cancer
Differences Between HER2 Positive and Negative Cancers
The presence or absence of HER2 overexpression has significant implications for breast cancer treatment. Patients with HER2 positive breast cancer often require targeted therapies that specifically address this genetic characteristic.
Statistics on HER2 Positive Breast Cancer Incidence
Approximately 20-25% of all breast cancers are classified as HER2 positive, making it a substantial subset within this disease category.
The Evolution of HER2 Positive Cancer Treatment
From Discovery to Treatment: A Historical Overview
Understanding the evolution of HER2 positive cancer treatment requires a look back at the early challenges and subsequent breakthroughs in addressing this specific type of cancer. Initially, healthcare providers faced significant obstacles in effectively targeting HER2 positive cancers. The lack of targeted therapies meant that conventional treatments often yielded limited success in managing the aggressive nature of these cancers.
However, the landscape of HER2 positive cancer treatment underwent a dramatic shift with the development of targeted therapies specifically designed to address the overexpression of HER2 neu protein. These breakthroughs revolutionized the approach to treating HER2 positive cancers, offering new hope to patients facing this challenging diagnosis.
The Role of Research in Advancing Treatment
Key studies have played a pivotal role in advancing the treatment options available for HER2 positive cancer. These studies have provided valuable insights into the underlying mechanisms driving HER2 positive cancers and have paved the way for innovative targeted therapies. By unraveling the complexities of HER2 overexpression, researchers have identified potential targets for intervention, leading to the development of novel treatment approaches.
Moreover, clinical trials have been instrumental in evaluating the efficacy and safety of emerging treatments for HER2 positive cancer. These trials provide essential data that informs healthcare providers about the most effective strategies for managing this specific type of cancer. Through rigorous testing and analysis, clinical trials contribute to expanding the armamentarium of treatment options available to patients with HER2 positive cancer.
Key Studies and Their Findings
Landmark studies investigating HER2 overexpression have elucidated its role as a key driver of aggressive tumor behavior. These studies have underscored the significance of targeting HER2 neu protein as a means to impede uncontrolled cell growth and proliferation characteristic of HER2 positive cancers. Furthermore, research findings have highlighted the potential synergistic effects when combining traditional chemotherapy with targeted HER2 blockade, leading to improved outcomes for patients.
The Importance of Clinical Trials
Clinical trials serve as an essential platform for evaluating novel therapeutic approaches tailored to address specific molecular characteristics such as HER2 overexpression. By enrolling participants in carefully designed studies, researchers can assess the safety and efficacy of experimental treatments while ensuring that patients receive optimal care. The data generated from these trials not only shapes current treatment standards but also lays the groundwork for future advancements in managing HER2 positive cancer.
Current Treatment Options and Their Effectiveness
As healthcare providers continue to advance their understanding of HER2 positive cancer, a range of treatment options has emerged to effectively manage this specific type of cancer.
Systemic Therapy: The Backbone of Treatment
Systemic therapy serves as the cornerstone of HER2 positive cancer treatment, encompassing various modalities aimed at targeting cancer cells throughout the body. This comprehensive approach often involves the use of chemotherapy in combination with HER2 blockade to impede the growth and proliferation of HER2 overexpressing cancer cells.
Chemotherapy plays a vital role in disrupting the rapid division of cancer cells, thereby inhibiting their ability to grow and spread. By administering cytotoxic agents, healthcare providers can effectively target rapidly dividing cells, including those characterized by HER2 overexpression. This approach aims to minimize the presence of cancer cells within the body, ultimately reducing the risk of disease progression.
In conjunction with chemotherapy, HER2 blockade therapies specifically target the overexpressed HER2 neu protein, hindering its proliferative effects on cancer cells. These targeted agents work by binding to the HER2 neu receptors on cancer cells, thereby impeding their ability to receive signals that promote uncontrolled growth. As a result, these therapies play a pivotal role in suppressing the aggressive behavior associated with HER2 positive cancers.
Targeted Therapy: A Closer Look at HER2 Neu Full Form Agents
Targeted therapy directed at the HER2 neu protein encompasses a diverse array of agents designed to specifically address this molecular characteristic. These targeted treatments include monoclonal antibodies such as trastuzumab and pertuzumab, which have demonstrated remarkable efficacy in inhibiting the proliferative effects of HER2 overexpression.
Moreover, small molecule inhibitors like lapatinib have shown promise in disrupting intracellular signaling pathways associated with HER2 positive cancers. By interfering with these pathways, these agents exert potent antitumor effects, ultimately contributing to improved outcomes for patients with this specific type of cancer.
A Multi-Modality Approach to Care
In addition to systemic therapies, a multi-modality approach involving surgery and radiation therapy is integral in managing HER2 positive breast cancer. Surgical intervention plays a crucial role in removing localized tumors and addressing any potential spread to nearby lymph nodes. By excising primary tumors and affected lymph nodes, surgeons aim to eliminate visible signs of cancer within the breast and surrounding tissues.
Furthermore, radiation therapy serves as an essential adjuvant treatment following surgery, targeting residual cancer cells that may remain after surgical resection. This localized approach aims to eradicate any remaining malignant cells while minimizing damage to healthy surrounding tissues.
Personalized Treatment Plans
Healthcare providers recognize the importance of tailoring treatment plans according to individual patient characteristics and disease attributes. Personalized approaches take into account factors such as tumor size, lymph node involvement, and overall health status when determining optimal therapeutic strategies for patients with HER2 positive breast cancer. By customizing treatment regimens based on each patient’s unique profile, healthcare providers strive to maximize treatment efficacy while minimizing potential adverse effects.
Prognosis and Future Directions
Understanding the Prognosis for HER2 Positive Cancer
When considering the prognosis for HER2 positive cancer, it is essential to examine the survival rates and the factors that influence outcomes. Survival rates for HER2 positive breast cancer have significantly improved in recent years due to advancements in targeted therapies and a better understanding of the molecular characteristics driving this specific type of cancer.
Survival Rates and Factors Influencing Outcomes
The prognosis for HER2 positive breast cancer is influenced by various factors, including the stage at diagnosis, tumor size, lymph node involvement, and the presence of hormone receptor status. Patients diagnosed at an early stage of HER2 positive breast cancer generally have more favorable outcomes compared to those with advanced-stage disease. Additionally, the effectiveness of treatment modalities such as surgery, chemotherapy, and targeted therapies plays a crucial role in determining long-term survival rates.
The Impact of Early Diagnosis
Early diagnosis of HER2 positive breast cancer significantly impacts patient outcomes. Detecting HER2 overexpression at an early stage allows healthcare providers to implement timely and effective treatment strategies aimed at eradicating cancer cells before they have the opportunity to spread beyond the breast and lymph nodes. As a result, early intervention can lead to more favorable prognoses and increased chances of long-term disease-free survival.
Innovations on the Horizon
As research continues to advance, several emerging treatments and therapies show promise in further improving outcomes for patients with HER2 positive breast cancer.
Emerging Treatments and Therapies
Ongoing research efforts have led to the development of novel therapeutic approaches tailored specifically to address HER2 overexpression. These emerging treatments encompass innovative targeted agents designed to further inhibit the proliferative effects of HER2 neu protein while minimizing potential adverse effects on healthy tissues. Additionally, immunotherapies targeting specific molecular pathways associated with HER2 positive cancers are being explored as potential avenues for enhancing treatment efficacy.
The Future of HER2 Positive Cancer Care
Looking ahead, the future of HER2 positive cancer care holds great promise with continued advancements in precision medicine and personalized treatment approaches. By leveraging cutting-edge technologies and harnessing a deeper understanding of tumor biology, healthcare providers aim to refine existing treatment paradigms while introducing next-generation therapies that further optimize patient outcomes. Moreover, ongoing clinical trials focused on identifying new therapeutic targets offer hope for expanding the armamentarium of treatment options available to patients with this specific type of cancer.
In summary, while challenges persist in managing HER2 positive breast cancer, ongoing research endeavors pave the way for innovative treatments that hold tremendous potential in shaping a brighter future for individuals affected by this disease.
Celnovte, a global leader in the research, development, and distribution of pathological diagnostic reagents and instruments, has made significant strides in the field of Immunohistochemistry and in-situ hybridization. Their advanced technologies, such as the MicroStacker™ IHC detection system, PolyStacker™ technology, and SuperISH™ RNA in-situ hybridization technology, have been instrumental in the accurate detection and diagnosis of various types of cancers, including HER2 positive cancer.
Moreover, Celnovte’s fully automated instrumentation, such as IHC stainers, H&E stainer, special stainer, cytopathology instrumentation, and digital slide scanner, have been installed in over 600 units globally since 2018. These tools have greatly enhanced the efficiency and accuracy of cancer diagnostics, contributing to the improved prognosis and treatment outcomes for patients with HER2 positive cancer.
With a network reaching over 1500+ top hospitals in China and over 10+ countries worldwide, Celnovte is committed to elevating precision in cancer diagnostics and enriching patients’ lives through their innovative products and services. Their mission aligns with the global effort to improve the curability of HER2 positive cancer and other types of cancer.
In conclusion, while HER2 positive cancer presents significant challenges, the advancements in diagnostic technologies, such as those developed by Celnovte, are playing a crucial role in improving detection, treatment, and potentially, the curability of this disease.