How Does HER2 Impact Breast Cancer Aggressiveness?

By admin
HER2, or Human Epidermal growth factor Receptor 2, is a protein that’s pretty important when it comes to controlling how cells grow and split up into ones! It’s part of a family of these receptors that hang out around the outside of cells in your body. And when we’re talking about breast cancer stuff here’s where things get interesting. HER2 is like a deal because it can act like a switch that turns things all wonky in your cells if something goes wrong with its gene or if there’s too much of it hanging around. That can then cause some trouble by making your cells grow out of control and playing a part in making breast cancer happen and get worse, over time. Healthcare providers and researchers must prioritize studying the behavior of HER2 and its influence, on treatment results.
Prevalence of HER2-Positive Breast Cancer
HER2-positive breast cancer makes up around 15 to 20 percent of all breast cancer cases. It’s known for its aggressive nature due to high levels of HER2 protein present in the cells. This form of cancer poses challenges in treatment as it requires targeted therapies tailored to its unique characteristics. High levels of HER2 can lead to clinical features in tumors necessitating specialized treatment options like immunotherapy which have shown promising results, in improving patient outcomes within this subtype. Being a factor, in breast cancer management and treatment planning involves recognizing the frequency of HER2 positive instances to customize individualized therapy approaches.
How Does HER2-Alter Cellular Behavior?
Mechanisms Behind Aggressiveness
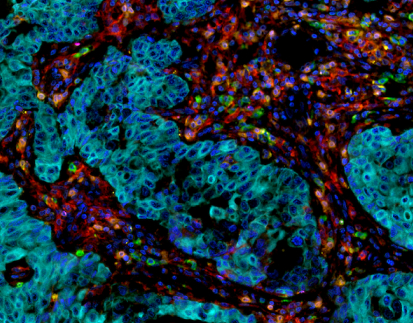
The mechanisms by which HER2 contributes to cancer aggressiveness are multifaceted. Mainly Overexpression of HER2 can result in increased signaling pathways that encourage cell growth and survival. This abnormal signaling impacts processes like the formation of new blood vessels and the spread of cancer cells to other parts of the body. Additionally, HER2 has been linked to the activation of cancer-causing pathways, such as PI3K-AKT and MAPK which contribute to further tumor growth and resistance, to programmed cell death. Therefore oncologists need to keep track of patients’ HER2 status because personalized treatment could greatly impact the progression of the disease.
Overexpression and Genetic Amplification
The overactivation or boost in the HER2 gene characterizes types of breast cancer specifically. If the gene is amplified genetically it leads to a rise in the quantity of HER2 proteins on the surface of cells. This enhances the signaling that fuels cellular behaviors. These cells display growth enlarged invasiveness and an increased likelihood of spreading to other parts of the body. Grasping how HER2 overexpression works serves not only as a way to diagnose but also as a gateway, to targeted treatments meant to block HER2 signaling. For accurate evaluation of HER2 amplification, using tools like the HER2 Gene Amplification Detection Kit is vital. This kit allows for precise detection of HER2 levels in tissue samples, aiding in the effective management of breast cancer.
Diagnosing HER2-Positive Breast Cancer
Common Symptoms of HER2-Positive Breast Cancer
Identifying the symptoms associated with HER2-positive breast cancer is crucial for timely diagnosis and treatment. Patients may present with various symptoms, such as a palpable lump in the breast, changes in nipple appearance, or unusual discharge. Additionally, symptoms may also include localized pain and swelling in the breast area. Awareness of these symptoms can lead to earlier diagnostic procedures, which is essential given the potentially aggressive nature of HER2-positive tumors.
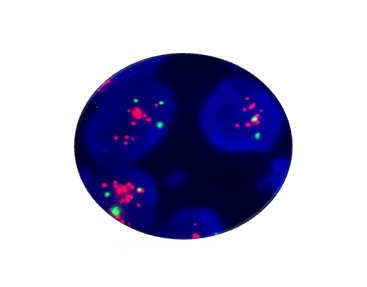
Diagnostic Techniques for HER2 Status
Accurate diagnosis of HER2 positivity involves various diagnostic techniques. The assessment of HER2 protein levels in breast cancer tissue often relies on Immunohistochemistry (IHC) a method used for this purpose. To provide a diagnosis when IHC results are inconclusive or ambiguous a supplementary examination such as Fluorescence In Situ Hybridization (FISH)might be conducted to detect HER2 gene amplification with greater accuracy. These diagnostic techniques play a role in guiding treatment decisions that could include targeted therapies, like trastuzumab. Healthcare professionals need to keep themselves informed about the recent developments, in diagnostic tools to guarantee that patients get the best possible care depending on their HER2-positive status.
Clinical Implications of HER2 Overexpression
The overexpression of HER2 significantly influences the prognosis and outcomes of breast cancer. Patients with HER2-positive variants often encounter more aggressive disease progression, with higher rates of metastasis. Studies indicate that these individuals have a poorer overall survival rate compared to those with HER2-negative breast cancer. Notably, the presence of HER2 alterations can dictate the treatment landscape as it often correlates with resistance to standard therapies. Identifying HER2 status early on can help in stratifying patients based on the aggressiveness of their cancer, allowing clinicians to tailor their approach.
Treatment Approaches for Early HER2 Positive Breast Cancer
The way we treat HER2-positive breast cancer patients has been changed greatly by targeted therapies like trastuzumab that have shown remarkable improvements in outcomes over time. Alongside trastuzumab are drugs, like pertuzumab and neratinib that are also being used to develop complete treatment plans. These treatments usually result in tumor response rates and lower chances of recurrence while enhancing the likelihood of survival. The integration of these targeted drugs with traditional therapies like chemotherapy reinforces the need for an initial HER2 status evaluation.
Why Early Detection Matters?
Detecting HER2 breast cancer early is crucial for successful treatment and better outcomes for patients. Having HER2 overexpression calls for action to slow down disease advancement. Research indicates that individuals, with stage HER2-positive breast cancer gain more from targeted treatment options by seeing significant decreases in tumor size and recurrence rates. Moreover, early identification enhances patient care strategies enabling healthcare providers to create tailored treatment approaches based on information. Enhanced screening processes and patient awareness initiatives are essential to promote early detection and subsequent interventions.
Why Choose Cutting-edge Detection Solutions?
Innovative Tools Like the HER2 Gene Amplification Detection Kit by Celnovte
Celnovte offers advanced diagnostic tools that empower healthcare professionals to accurately assess HER2 status, particularly through the HER2 Gene Amplification Detection Kit. This new approach makes use of state-of-the-art technology to accurately identify HER2 gene amplification in tissue samples. By incorporating this tool into processes doctors can enhance the precision of their diagnoses and provide personalized treatment plans for each patient. Improved accuracy in diagnosis can have an effect, on patient care outcomes by enabling timely and suitable interventions.
Comprehensive Diagnostic Support with Celnovte
Celnovte is committed to providing comprehensive diagnostic support to healthcare professionals dealing with HER2-positive breast cancer. Their advanced testing methodologies and thorough analysis capabilities offer a robust platform for assessing tumor characteristics. Celnovte’s resources are designed to support clinicians in every step of the diagnostic process, from initial assessment to treatment planning. By utilizing Celnovte’s platforms, practitioners can ensure they deliver the highest level of personalized care while keeping pace with the evolving landscape of breast cancer treatment.
Emerging Treatments for HER2 Positive Breast Cancer
In the past few years, there have been major strides in specialized treatments for HER2-positive breast cancer patients focusing on HER2-positive breast cancer treatments. Numerous studies have investigated drugs to combat HER2 activation. These advancements have led to the introduction of dual treatment plans that combine therapies targeting HER2 with pathways involved in tumor development. Furthermore, research, on antibody-drug combinations has shown outcomes by improving the direct delivery of cytotoxic drugs to cells that overexpress HER2. The advancements in this treatment choice highlight the significance of regularly checking HER2 status to enhance treatment results effectively.
Personalized Medicine Approach
The advancements in medicine have significantly transformed the way HER2-positive breast cancer is treated. With treatment plans tailored to suit tumor characteristics like HER levels of expression the effectiveness of therapy is increased. This methodology enables healthcare providers to choose the targeted medications potentially along with chemotherapy or immunotherapy to reduce side effects and maximize results. Ongoing studies into the molecular features of tumors equip healthcare providers, with better tools to anticipate how patients will respond to treatment and adjust care plans accordingly. The ongoing advancements, in personalized healthcare are significantly influencing the direction of breast cancer care and control strategies.