ER Positive and ER Negative What Every Expert Needs to Know
 2024-10-22
2024-10-22
By admin
ER positive breast cancer is characterized by the presence of estrogen receptors on the surface of the tumor cells. In this context, estrogen plays a significant role in promoting the growth of these cancer cells. Tumors that are ER positive tend to exhibit a slower growth rate compared to their ER negative counterparts and may respond positively to hormone therapies aimed at blocking estrogen from fueling tumor growth.
Characteristics of ER Positive Tumors
ER positive tumors display unique characteristics, including a higher likelihood of being detected at an earlier stage and a better overall prognosis in some cases. The majority of these tumors are diagnosed in postmenopausal women, although they can affect individuals at any age. The higher incidence of ER positive breast cancers signifies the importance of establishing targeted treatment plans that include hormone receptor testing as part of the diagnostic process.
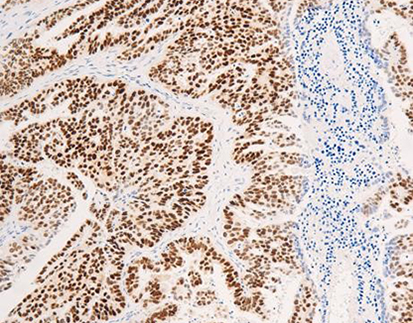
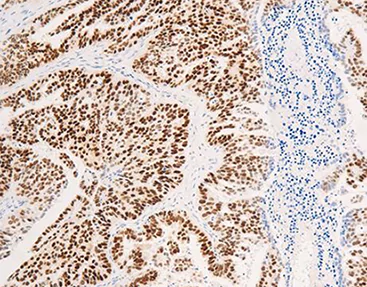
Diagnostic Techniques for ER Positive Breast Cancer
Diagnostic techniques for ER positive breast cancer generally include hormone receptor testing, which can be conducted via immunohistochemistry (IHC) to determine the presence of estrogen receptors. Alongside imaging techniques, such as mammography and ultrasound, pathologists analyze biopsy specimens to assess tumor markers and establish the status of the ER. Accurate diagnostic assessments are crucial for determining the appropriate treatment protocol and improving patient outcomes. For those investigating personalized medicine options, exploring the nuances of hormone receptor status can lead to better-targeted therapies.
How Does ER Negative Breast Cancer Differ?
When discussing ER negative breast cancer, it is important to note that these tumors do not have estrogen receptors on their cellular surfaces. This absence suggests a different biological behavior and treatment response compared to ER positive tumors. ER negative breast cancer is often more aggressive and may present with a higher prevalence of metastasis at diagnosis.
Understanding ER Negative Tumors
ER negative tumors are associated with distinct clinical and pathological features such as higher grade tumors, lack of differentiation, and a more advanced stage at diagnosis. The treatment options available for ER negative breast cancer involve chemotherapeutic regimens and targeted therapies, as opposed to relying on hormone therapies that are effective in ER positive cases. Understanding the biological behavior of these tumors assists clinicians in formulating a diligent approach to patient care.
Diagnostic Methods for ER Negative Breast Cancer
For diagnosing ER negative breast cancer, similar techniques as those used for ER positive tumors are employed, with a focus on the absence of hormone receptors. Immunohistochemistry remains critical, along with additional molecular profiling that may help identify alternative pathways being utilized by the tumor for growth and spread. Histopathological assessments play a significant role in this process, as they inform the identification of tumor subtypes that require specialized treatment strategies. Proper diagnosis enables oncologists to personalize treatment plans effectively and optimize patient outcomes.
What Are the Treatment Strategies for ER Positive and ER Negative Breast Cancers?
Treating ER positive and ER negative breast cancers necessitates distinct approaches due to their differing biological characteristics and growth mechanisms. Understanding these treatment strategies plays a vital role in enhancing overall patient care and aligning therapeutic options with tumor biology.
Therapeutic Approaches for ER Positive Cases
For ER positive breast cancer, therapeutic strategies often incorporate hormone therapies such as tamoxifen or aromatase inhibitors, which work to block estrogen’s effects on the tumors. These treatment options can lead to significant reductions in recurrence rates and improve survival chances. Additional strategies may involve targeted therapies designed to enhance the effectiveness of other treatment modalities. Combining hormone therapy with chemotherapy can be beneficial in certain aggressive cases, allowing for a more comprehensive treatment plan.
Treatment Paradigms for ER Negative Cases
In contrast, the treatment paradigm for ER negative breast cancer generally focuses on chemotherapy and newer targeted therapies that do not involve hormone receptor interaction. Regimens may include anthracyclines and taxanes, or a combination thereof, depending on the tumor’s biology and stage. Ongoing clinical trials explore additional targeted therapies that may further refine treatment options for this group. Leading a multidimensional approach to treatment through discussions on clinical trials, such as those offered at Celnovte, may provide patients with promising alternatives and ways to manage their diagnosis effectively.
In conclusion, the difference between ER positive and ER negative breast cancer is crucial for professionals in the field. While hormone receptor status guides treatment strategies, advancements in diagnostic techniques and therapeutic options continue to evolve, ensuring improved patient care.
For those seeking a deeper exploration of potential solutions, visiting the solution center can offer insights into how to approach specific challenges associated with breast cancer treatment. For additional information on estrogen receptors, refer to this link on Estrogen Receptor (ER). Moreover, professionals may wish to view Solutions that provide further resources and expertise.
Why Is Accurate Diagnosis Critical in Managing Breast Cancer?
Accurate diagnosis is essential in managing breast cancer, particularly when discerning between ER positive and ER negative subtypes. Misclassification can lead to inappropriate treatment decisions, potentially impacting survival rates and patient quality of life. Specialists must rely on precise testing methodologies, such as immunohistochemistry and molecular profiling, to ascertain the receptor status of tumors. This process helps in stratifying patients into suitable treatment categories, facilitating personalized medicine approaches that align with the biological characteristics of their cancer.
Consequences of Misdiagnosis
The ramifications of misdiagnosis in breast cancer can be severe. Incorrectly labeling a tumor as ER positive when it is actually ER negative may lead to ineffective treatments, such as hormone therapy, which would not address the aggressive nature of ER negative cancer. This can result in unnecessary side effects, increased tumor progression, and lowered survival rates for the patient. Additionally, such errors can foster a sense of mistrust in healthcare systems, impacting patient adherence to treatment protocols and overall health outcomes.
Advances in Diagnostic Technologies
Our knowledge about ER status has greatly benefited from advancements in diagnostic technologies. Next-generation sequencing and liquid biopsies are transforming how oncologists approach breast cancer diagnostics. These innovative methodologies allow for a more comprehensive understanding of tumor biology and enable the detection of mutations that influence therapy response. As these technologies continue to evolve, they promise to improve diagnostic accuracy further, helping to ensure that treatment regimens are tailored more closely to individual patient needs.
Solutions and Innovations in Therapy Management
Effective therapy management hinges on a robust understanding of the distinctions between ER positive and ER negative breast cancer. Tailoring treatment based on receptor status allows oncologists to implement solutions that optimize outcomes. As the landscape of cancer therapy expands, novel combinations of therapies are being explored, enhancing efficacy while minimizing adverse effects. Implementing best practices in managing these cancer subtypes can lead to substantial improvements in patient care.
How Do Clinical Trials Influence Our Knowledge on ER Status?
Clinical trials play a pivotal role in advancing our understanding of breast cancer, particularly regarding ER status. They provide critical data that influence treatment protocols and inform clinical practice guidelines across the field. Well-designed trials assess the efficacy of various treatment regimens, allowing insights into how ER status affects response rates and long-term outcomes. By analyzing patient outcomes within these trials, researchers can gather vital information that shapes future therapeutic approaches for both ER positive and ER negative breast cancers.
Recent Findings in ER Positive Research
Recent studies focusing on ER positive breast cancer have revealed encouraging trends regarding treatment and management strategies. Emerging data suggest that the use of targeted therapies in conjunction with traditional hormone therapies may enhance treatment outcomes significantly. For instance, combining aromatase inhibitors with CDK4/6 inhibitors has shown promise in reducing recurrence rates and improving survival in this patient population. Additionally, trials have explored the impact of genetic testing in guiding therapy decisions for ER positive patients, tailoring strategies based on individual risk profiles.
Emerging Insights from ER Negative Studies
Conversely, research on ER negative breast cancer has identified unique pathways that guide therapy management for this subtype. Studies have highlighted the importance of biomarker-driven therapies, particularly those targeting pathways unrelated to hormone receptor interactions. Agents such as PARP inhibitors and immunotherapy are being investigated for their potential roles in treating ER negative tumors. By examining resistance mechanisms and identifying novel targets, ongoing research aims to enhance therapeutic effectiveness and ultimately improve prognosis for individuals diagnosed with ER negative breast cancer.
In summary, detailed comparisons between ER positive and ER negative breast cancer are critical for experts navigating treatment protocols. As research progresses, maintaining awareness of how these developments impact clinical practice will help ensure optimal patient care. For a deeper exploration of potential solutions in breast cancer management, consider visiting the Solutions center. For further insights on estrogen receptors, you can view more through the Estrogen Receptor (ER) resource.
RELATED PRODUCTS