Case Study丨Application of CELNOVTE Intraoperative Rapid Immunohistochemistry in the Diagnosis of Bronchiolar Adenoma and Lung Adenocarcinoma

By celnovte
Patients with pulmonary bronchiolar adenoma (BA) usually have no obvious clinical symptoms, and almost all diagnoses are first discovered via CT scan images. However, since BA imaging manifestations are difficult to differentiate from early malignant tumors, intraoperative frozen section pathology diagnosis is a necessary step [1].
Because the peripheral lung tissue of proximal BA is often rich in mucus cells, it needs to be distinguished from invasive mucinous adenocarcinoma. Distal BA luminal cells lack mucin and ciliated cells, or even only Clara or alveolar cells, so they are easily confused with non-mucinous adenocarcinoma in situ, minimally invasive adenocarcinoma, or even invasive adenocarcinoma. Due to the unclear cell ciliary structure on frozen sections, the interstitium is widened and it is difficult to determine whether there are basal cells, which can easily be confused with invasive mucinous adenocarcinoma and well-differentiated acinar adenocarcinoma, leading to misdiagnosis [2-3].
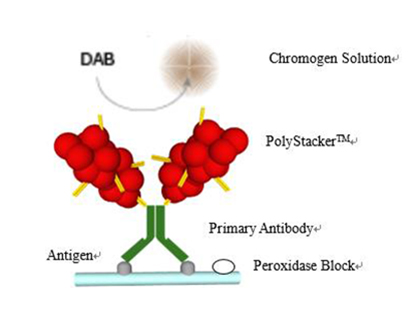
Immunohistochemistry to determine the presence of continuous basal cells is an important basis for diagnosis. Intraoperative rapid immunohistochemistry for CK5/6 and other antibodies can assist in differential diagnosis.
Clinical information:
The patient was a 65-year-old female. The frozen section (nodule in the lower lobe of the left lung) showed a gray-white nodule with a diameter of 1 cm.
01 Intraoperative H&E staining:

For lesions with a clear boundary around the bronchus in lung tissue, columnar/cuboidal epithelium can be seen growing in adenoid, papillary or adherent form, and it is necessary to differentiate between invasive carcinoma and bronchiolar adenoma.
02 Intraoperative rapid immunohistochemistry

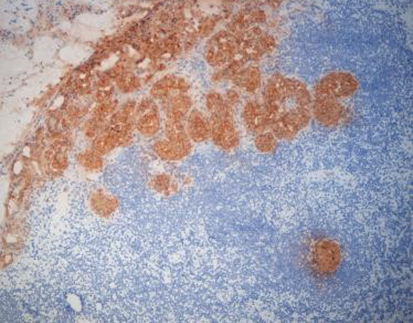
Intraoperative rapid immunohistochemistry on frozen sections for CK5/6 (-) showed no basal cells, consistent with invasive adenocarcinoma.
03 Postoperative H&E staining

The postoperative paraffin H&E staining results were consistent with the intraoperative staining results.
04 Postoperative immunohistochemistry
Paraffin section immunohistochemistry for p40-, TTF-1+, Napsin A(+).
p40 negative

TTF-1 positive

Napsin A positive

Diagnostic result:
The final diagnosis based on histomorphology and immunohistochemistry: invasive adenocarcinoma, non-mucinous type, moderately differentiated.
Further Content – Statistics Based Evidence for the Efficacy of Interoperative Rapid IHC
At present, intraoperative frozen section H&E staining technology is an important means to quickly determine the nature of specimen lesions during surgery and guide the surgical method and scope. However, the morphology of tissue cells in some diseases is relatively similar, making it difficult to identify by H&E staining alone. It is easy to miss or misdiagnose, and even cause Patient’s secondary surgery or medical accident.
Han, Liyuan et al.[4] conducted a comparative analysis of the pathological diagnosis results of intraoperative frozen sections and postoperative paraffin sections and immunohistochemistry pathology diagnosis results. They found that the accuracy of intraoperative frozen section pathological examination in differential diagnosis of benign and malignant pulmonary nodules was 99.2. %, and the accuracy of classifying lung malignant tumors was 85.3%.
Shen, Yuanlong et al. [5] used paraffin section immunohistochemistry confirmed pulmonary sclerosing pneumonitis (PSP) and lung adenocarcinoma tissues as the research subjects. By comparing the TTF-1, ER and Ki-67 expression, it was found that the diagnosis accuracy of intraoperative rapid immunohistochemistry and intraoperative H&E staining for PSP were 100.00% and 58.33% respectively, and the accuracy for diagnosing lung adenocarcinoma were 96.15% and 76.92% respectively (Table 1). This indicates that rapid intraoperative frozen section immunohistochemistry can significantly improve the accuracy of diagnosis of PSP and lung adenocarcinoma. Furthermore, by comparing the differential expression results of TTF-1, ER and Ki-67 in the two diseases, it was found that they can be used as indicators of rapid intraoperative frozen section immunohistochemistry for differential diagnosis of the two diseases.
Table 1 – Comparison of the accuracy of intraoperative frozen section rapid immunohistochemistry and H&E staining in the diagnosis of PSP and lung adenocarcinoma

Note: * P<0.05, Fisher’s exact test
In addition, a comparison of the rapid immunohistochemical staining results of intraoperative frozen sections and the immunohistochemical staining results of paraffin sections showed that there was no significant difference between the two. This confirms that rapid immunohistochemical staining of intraoperative frozen sections has practical clinical significance for the differential diagnosis of PSP and lung adenocarcinoma.
Intraoperative frozen section rapid immunohistochemistry is performed simultaneously with intraoperative frozen section H&E staining. A report is issued within 30 minutes after the specimen is received in the pathology department, which does not affect the reporting time of frozen diagnosis. At the same time, not only can intraoperative rapid frozen section immunohistochemistry improves the accuracy of diagnosis, it can also significantly shorten the patient’s pathological waiting time and provide a reliable basis for adjusting the surgical plan.
References:
[1] WANG Yingxia; TIAN Yang; ZHAO Wen; ZHANG Xuan. Clinicopathological analysis of 24 cases of bronchiolar adenoma. Journal of Clinical and Pathological Research. 2023,43(05):880-887. (in Chinese)
[2] Liu S, Liu N, Xiao M, Wang L, Wang EH. First case of bronchiolar adenoma lined purely by mucinous luminal cells with molecular analysis: A case report. Medicine (Baltimore). 2020 Sep 25;99(39):e22322.
[3] ZHU Hao-hao; REN Guang-yu; WEN Jian-feng. Several benign pulmonary diseases easily misdiagnosed during intraoperative frozen sections. Chinese Journal of Diagnostic Pathology. 2023,30(07):701-703, 707. (in Chinese)
[4] HAN Liyuan; CUI Yayan; CHEN Dong; MEI Shaoshuai; LIAN Guoliang. Study on pathological diagnosis of pulmonary nodules in frozen operation. Journal of Cardiovascular and Pulmonary Diseases. 2022,41(03):302-305, 308. (in Chinese)
[5] SHEN Yuanlong; LI Lin; WU Zihao. Comparison of the application of intraoperative frozen section rapid immunohistochemistry and HE staining in the diagnosis of sclerosing pneumoma and lung adenocarcinoma. Anhui Medical Journal. 2019,40(12):1392-1395. (in Chinese)