p16/Ki-67 Dual-staining Cytology in Cervical Cancers
Cervical cancer is the fourth most common malignant tumor among women worldwide. and the infection of human papillomavirus (HPV) is essential cause. Certain HPV types, in particular high-risk HPV (HR-HPV) 16 and 18, may lead to cervical dysplasia, reversible forms of precancerous lesions. Early diagnosis through various screening techniques is the main step in the prevention and treatment of cervical cancer. At present, three main methods, cytology, HPV testing, and cytology combined with HPV testing, have been applied to cervical cancer screening.
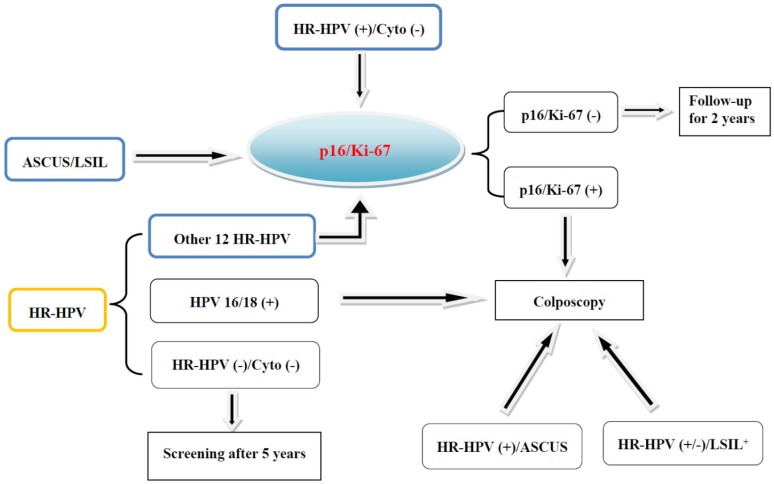
According to the FDA guidelines for primary HPV screening, women with positive HPV16 or HPV18 were immediately examined by colposcopy, while women with positive HPV but negative HPV16 or HPV18 were examined by cytology. If cytology is negative, they will be followed up 12 months later. Many women with positive HPV need repeated cytological follow-up because of the relatively low sensitivity of cytology. Therefore, more effective markers are required to triage HPV-positive women with normal cytology or negative HPV16/18 and to identify women with potential high-grade CIN from cytological ASCUS/LSIL candidates. Accumulating evidence suggests that p16/Ki-67 dual-staining cytology is becoming an alternative biomarker, showing overall high sensitivity and specificity for identifying high-grade CIN.
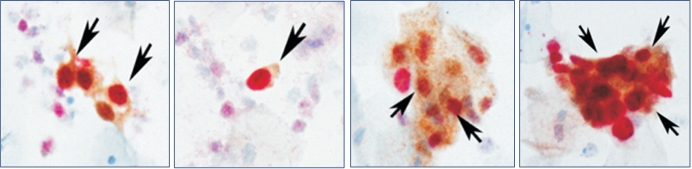
p16 is a tumor suppressor and Ki-67 is a cellular marker for proliferation. The over-expression of p16 and expression of Ki-67 under physiological situations are mutually exclusive and do not occur in the same cervical epithelial cell. Therefore, the p16/Ki-67 co-expression implies deregulation of the cell cycle induced by HR-HPV and detection of p16/Ki-67 co-expression can serve as a marker to predict the cell transformation by HR-HPV and the presence of high-grade CIN lesions. Co-expression of p16/Ki-67 can be detected with antibodies against p16 and Ki-67. The brown cytoplasm/nuclear signal was displayed by p16 staining alone, and the red nuclear signal was displayed by Ki-67 staining alone. Positive p16/Ki-67 dual-staining cells had brown cytoplasm signals for p16 expression, and dark red to red brown nuclear signals reflected the co-localization of p16 and Ki-67 in the same cell.
Dual staining positive cells: the cytoplasm stained brown yellow and the nucleus stained red (marked by the arrow)
https://www.celnovte.com/p16-ki-67-detection-reagent-kit-immunocytochemistry-2/
The results of HPV infection vary greatly, and follow-up of HPV-positive women is complicated and laborious. To eliminate the unnecessary follow-up, HPV-positive women need a timely triage. Cytology is usually used to triage HPV-positive women who are negative for HPV16 or 18. Increasing studies have shown that p16/Ki-67 dual-staining is useful for the triage of HPV-positive women.
p16/Ki-67 dual-staining cytology is of great significance in screening and triaging of cervical cancer and precancerous lesions. It provides a good risk marker for the stratification of HPV-positive women, including normal cytological patients, and for the identification of high-grade CIN from women diagnosed as ASCUS or LSIL. Compared with Pap cytology and HPV detection, it has higher sensitivity and specificity in detecting cervical precancerous lesions and cervical cancer. This is also helpful for the diagnosis of cervical glandular lesions. The combination of p16/Ki-67 dual-staining and HP-HPV detection is recommended as a strategy for monitoring women treated for high-grade CIN.
Refernce: Application of p16/Ki-67 dual-staining cytology in cervical cancers by Li Yu, Lingyan Fei, Xubin Liu, Xufang Pi, Liantang Wang , Shangwu Chen
Related News






 2021-05-12
2021-05-12